MDMA-assisted psychotherapy as a potential treatment for alcoholism, by Dr Ben Sessa
MDMA has been studied successfully in the last 30 years as a treatment for PTSD. The MDMA non-ordinary state of consciousness allows the user to safely address painful emotional memories that would normally be avoided. Often patients with PTSD have had early childhood traumatic experiences. My experience as a child and adolescent psychiatrist working with abused and maltreated children has shown me how unresolved childhood trauma frequently develops into adult disorders, particularly addictions. In recent years, my work with adult patients with addiction has shown the huge difficulty in treating alcoholism because patients often cannot address and resolve their childhood issues. As a result, modern psychiatry’s success rate at treating alcoholism is very poor, not much better than in Victorian times: 90% of patients will return to drinking within four years after detox and the best available treatment.
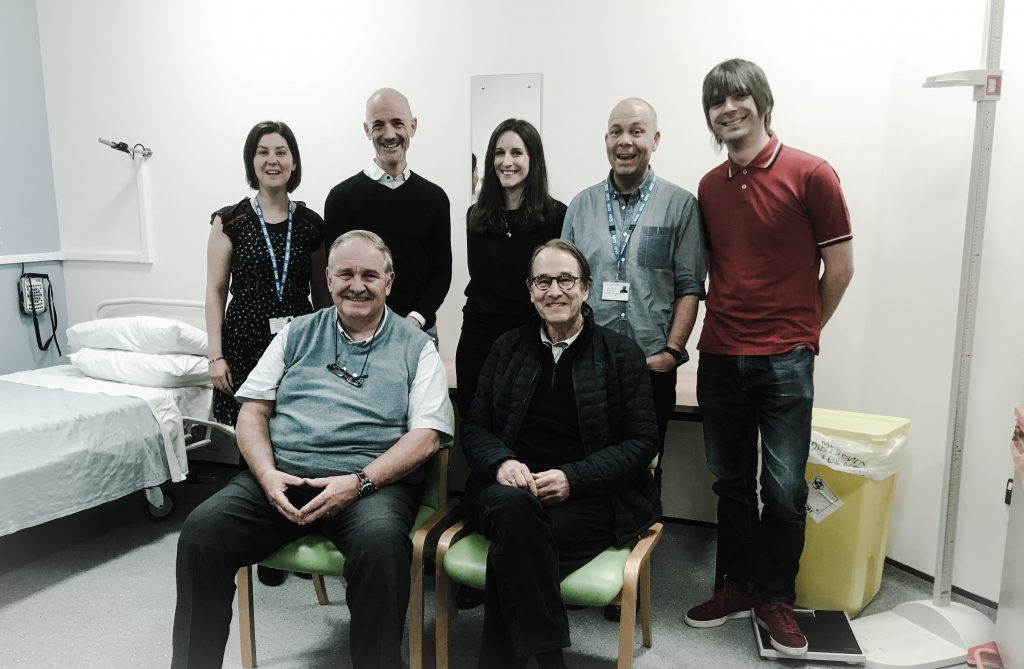
We are currently running a small, open-label proof-of-concept feasibility study to prove the safety and tolerability of MDMA-assisted psychotherapy in Bristol. The project is affiliated with Bristol University and Imperial College, London, who are sponsoring the study. Our aim was to treat twenty patients with a diagnosis of alcohol use disorder using an eight-week course of MDMA-assisted psychotherapy, which entails taking MDMA twice during the course of the eight-week therapy, spaced between non-drug preparation and integration therapy sessions.
This led our team in Bristol to develop a study exploring MDMA-assisted psychotherapy as a treatment for alcoholism. While classic psychedelic drug-assisted psychotherapy (e.g., with LSD and psilocybin) has a rich history in the treatment of addiction, ours is the world’s first study to explore MDMA-assisted therapy for the treatment of any addiction. The rationale is that, since trauma so often underlies addiction and MDMA appears to be effective at treating trauma, MDMA therapy could be useful for treating alcoholism.
Myself and co-therapist Dr Laurie Higbed, an addiction clinical psychologist, are carrying out the psychotherapy sessions. The main outcome measures are the safety and tolerability of this form of drug-assisted psychotherapy for patients with alcohol use disorder. All patients are screened according to strict inclusion and exclusion criteria for eligibility. We monitor physiological observations throughout the MDMA sessions and for seven days after each MDMA session. We see them for eight weeks during the therapeutic course, and then for nine months of follow-up after the therapeutic course to collect outcome data. We assess drinking behaviour and other measures include participants’ mental health, physical health, quality of life, sleep, and suicidal status
So far, we have fifteen patients fully enrolled and we have carried out twenty-six MDMA-assisted psychotherapy sessions. Results are promising, with participants reporting MDMA effects of profound significance. It appears MDMA-assisted psychotherapy helps to unlock rigid, maladaptive, addictive behaviours and support a move towards recovery. There have been no serious adverse events and patients report finding the course to be safe and tolerable, far superior to previous attempts at tackling their lifelong alcoholism. So far, of the thirteen patients who have completed the therapeutic course, only two have returned to their full levels of drinking that they presented with at the start of the course. The project aims to run until December 2019. Thereafter, the Bristol-Imperial MDMA-for-Alcoholism team hope to progress to a placebo-controlled randomised study.
Due to MDMA’s status as a Schedule 1 drug, we have encountered enormous financial and regulatory hurdles in setting up this project. The costs of obtaining Schedule 1 licences at multiple sites and overcoming regulatory hurdles associated with obtaining clinical-grade MDMA have impacted our progress. The current scheduling of MDMA under the Misuse of Drugs Regulations is significantly impairing its clinical research. In total, including manufacturing costs, approval certificates, transport, storage, encapsulation, pharmacy, and dispensing costs, our MDMA is costing the study approximately £9,000 per gram. This prohibitive cost, due primarily to its Schedule 1 status, puts off many would-be researchers and seriously hampers advances in this vital field of medical research, which could have enormous benefits for a large population of patients for whom current traditional clinical treatments are sadly often ineffective.
Podcast
- All
Links
- All
Support
- All
BIPRP
- All
Science Talk
- All
Amanda's Talks
- All
- Video Talk
- Featured
- 2016 Onwards
- 2011-2015
- 2010 and Earlier
- Science Talk
- Policy Talk
One-pager
- All
Music
- All
Amanda Feilding
- All
Events
- All
Highlights
- All
Psilocybin for Depression
- All
Current
- All
Category
- All
- Science
- Policy
- Culture
Substance/Method
- All
- Opiates
- Novel Psychoactive Substances
- Meditation
- Trepanation
- LSD
- Psilocybin
- Cannabis/cannabinoids
- Ayahuasca/DMT
- Coca/Cocaine
- MDMA
Collaboration
- All
- Beckley/Brazil Research Programme
- Beckley/Maastricht Research Programme
- Exeter University
- ICEERS
- Beckley/Sant Pau Research Programme
- University College London
- New York University
- Cardiff University
- Madrid Computense University
- Ethnobotanicals Research Programme
- Freiburg University
- Medical Office for Psychiatry and Psychotherapy, Solothurn
- Beckley/Sechenov Institute Research programme
- Hannover Medical School
- Beckley/Imperial Research Programme
- King's College London
- Johns Hopkins University
Clinical Application
- All
- Depression
- Addictions
- Anxiety
- Psychosis
- PTSD
- Cancer
- Cluster Headaches
Policy Focus
- All
- Policy Reports
- Advisory Work
- Seminar Series
- Advocacy/Campaigns
Type of publication
- All
- Original research
- Report
- Review
- Opinion/Correspondence
- Book
- Book chapter
- Conference abstract
- Petition/campaign
Search type
