
Why Science Needs Psychedelics: A Paradigm Shift for Psychiatry
In the UK, 1 in 4 people are affected by mental illness. 1 in 3 teenage girls suffer from an anxiety or depressive disorder, and suicide is the leading cause of death among the young. Nearly 50% of the population will develop a mental health disorder at some point during their lifetime, and the World Health Organisation has declared that depression is the leading cause of disability. Mental illness costs the UK economy an estimated £100 billion pounds every year.
The number of antidepressants prescribed in England has more than doubled in the last decade, with the most common treatment being SSRIs. Of the 30% of patients who receive no benefit from current pharmacological treatment, up to 15% will go on to kill themselves.
Against this backdrop, it is surprising that no major breakthrough in drug development for depression and other psychological disorders has happened in the past three decades, since the discovery of SSRIs.

Dozens of species of mushrooms naturally produce the psychedelic compound psilocybin.
In the last 20 years, research from the Beckley Foundation and others has found that psychedelics, such as psilocybin – the psychoactive ingredient in magic mushrooms – can produce dramatically higher rates of efficacy than any other available treatments. As tools to aid psychotherapy, they work immediately, after a single or a few doses, with benefits lasting weeks, months and maybe years, with no negative or long-term side-effects.
As part of the Beckley/Imperial Psychedelic Research Programme, in 2016 we investigated the effects of psilocybin-assisted psychotherapy in treatment-resistant depression. The patients we recruited had suffered from moderate-to-severe depression for an average of eighteen years, and had received no relief from conventional medicines or psychotherapy. A first session with a small dose of psilocybin confirmed that the compound was well-tolerated by each patient. In another session shortly after, a larger dose – with more intensely felt psychoactive effects – was given. Two clinicians stayed with the patients in a softly lit, comfortable room, allowing the patients to experience a mostly uninterrupted journey, with occasional ‘check-ins’ to make sure they were doing well.

A therapy room used in the Beckley-Imperial study of psilocybin-assisted psychotherapy for treatment-resistant depression
A week after the second session, all patients showed a reduction in depression severity, with 67% of them meeting criteria for complete remission. These impressive results were robust over time: at three-months 42% of all patients remained depression-free, and more than half displayed significant improvements in depression severity relative to their pre-psilocybin scores.
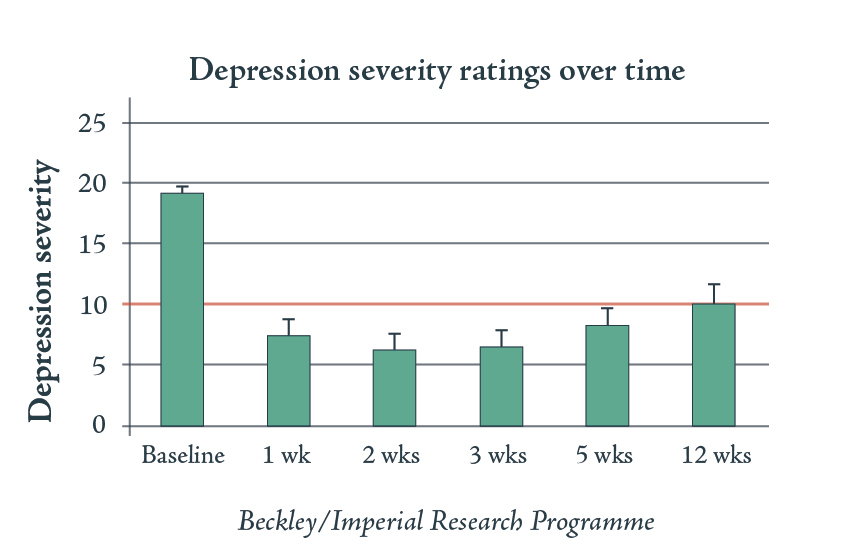
Two sessions of psilocybin-assisted psychotherapy produced robust effects on treatment-resistant depression. A score of more than 10 on the QIDS-SR 16 is the threshold for moderate depression
Since the 1960’s I have been greatly interested in the mechanisms underlying the changing states of consciousness brought about by psychedelics. Our fMRI studies with psilocybin and LSD investigated the changes in blood supply within the brain as well as neuronal connectivity. In doing so we have begun to reveal the mechanisms underlying the significant promise of these compounds as tools to aid psychotherapy.
One of the most striking effects we observed was a decrease in blood supply and thus activity within the Default-Mode Network (the DMN), a collection of widespread brain regions that work together to coordinate the activity of diverse areas of the brain, in doing so controlling our conscious experience and maintaining our sense of self. When the DMN disintegrates under LSD or psilocybin, the inhibitory control it normally exerts over the other areas of the brain weakens, allowing for a dramatic increase in global connectivity, allowing regions to communicate with distant partners with which they typically do not talk. As well as producing the subjective experience of ‘ego dissolution’, this process leads to the emergence of a more complex, less predictable, and more flexible state of consciousness. In this more fluid, ‘plastic’ state, long-lasting changes can take place, repressed memories can be accessed, and the maladaptive thought processes of depression and other psychological disorders can be reset, like a computer being rebooted.
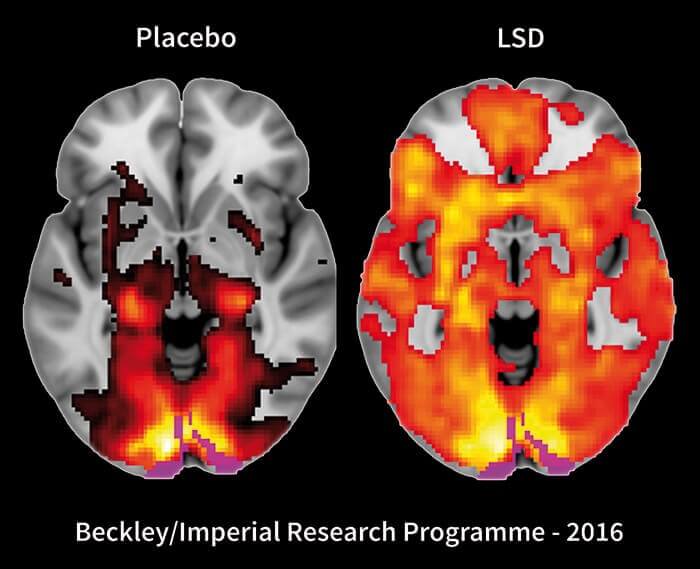
Taking LSD leads to a transient increase of global functional connectivity in the brain, with more communication between networks that are usually separate
The potential for psychedelic-assisted psychotherapy does not stop at treating depression. Dysfunction of the DMN is implicated in a whole host of other mental health conditions, including addiction, obsessive-compulsive disorder, anxiety, and PTSD, among others. What characterises them all is an excessive pattern of thought or behaviour becoming rigid and entrenched, almost impossible to break out of despite an awareness of their destructiveness. An experience of a ‘peak state’, brought about by a psychedelic, provides a chance for an individual to see the inner self and the outer world afresh, affording an opportunity to begin anew.
Although a deeper understanding of the brain mechanisms underlying this treatment has only been made possible by modern neuroimaging techniques, the potential for psychedelics to heal in this way is not a recent discovery. LSD was considered a wonder-drug when it first appeared in the 1950’s. Hundreds of published papers and thousands of patient reports testified to its promise for new treatments for a wide range of illnesses. A recent meta-analysis of the best-controlled studies conducted in the 1960’s using LSD for alcohol use disorder – a condition which, to this day, has notoriously poor treatment outcomes– found a single session to be more successful in treating alcohol dependence than daily doses of acamprosate or naltrexone, our current go-to pharmacological interventions. Bill Wilson, the founder of Alcoholics Anonymous, wanted to include LSD-therapy in the treatment programme for alcohol dependence, understanding that the subjective effects of LSD – which we now know to be caused by the disintegration of the DNM and an increased plasticity of the brain state– can help to achieve a change in perspective that allow recovery to begin.
Psychedelic-assisted psychotherapy can create a truly revolutionary paradigm-shift in psychiatry. This is not some far-off medical advance visible on the horizon, awaiting some technological breakthrough before becoming feasible. Psychedelic-assisted therapy could be made available in clinics right away, were it not for repressive regulation. But the psychedelics remain among the most heavily restricted compounds in the world: in the UK, they are Class A, Schedule 1 drugs under the Misuse of Drugs Act (1971) and Misuse of Drugs Regulations (2001). Both classifications categorise the psychedelics as having no medical use, as well as being extremely dangerous.
It is now clear that both of these accusations are demonstrably untrue. The foregoing examples provide a brief introduction to their therapeutic potential. Our studies have found that, when administered by skilful clinicians in controlled environments, psychedelics present no significant risk and are not addictive. Meanwhile, recent population studies –analysing information from more than 120,000 people – have found no link between psychedelic use and mental health problems.
Modern psychiatry is failing huge numbers of people. The research undertaken in the last decade has suggested many areas where psychedelics could be invaluable for alleviating the suffering of mental health issues. And yet, further research is constantly obstructed by legislation that makes it prohibitively expensive, extremely time-consuming, or impossible for researchers to access the materials we need at affordable prices.
The hesitance of some towards reforming these regulations is easily enough understood. An entire generation has been told that psychedelics are harmful to health, that they are toxic and dangerous. But a more informed attitude is possible – indeed it is already endorsed by many, if not most. The potentially deadly opiate family contains morphine, a useful painkiller. Amphetamines can be prescribed as a treatment for ADHD, or become a drug of potential abuse when taken recreationally as a stimulant. With the appropriate clinical oversight, a compound’s therapeutic benefits can vastly outweigh its risks. By moving psychedelics from Schedule 1 to Schedule 2, where morphine and amphetamines currently sit, doctors can prescribe them to those in need, and further research can be carried out much more easily.
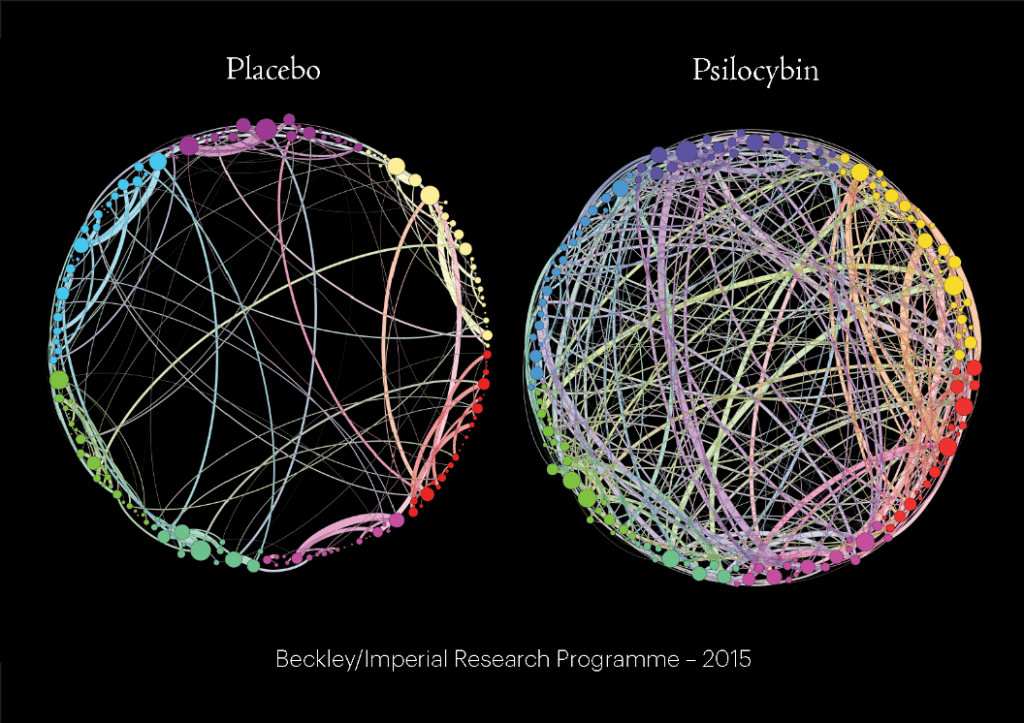
Under the influence of the psychedelic compound psilocybin, the functional connectivity of our brains increases, with brain regions communicating much more than usual with other networks
Our approach to these drugs has so far been characterised by patterns of thought and behaviour that have become rigid and entrenched, hard to break out of despite an awareness of their destructiveness. Let us put health, and the reduction of suffering ahead of political expediency and rigid-thinking: the time to act is now.
Words: Amanda Feilding
Podcast
- All
Links
- All
Support
- All
BIPRP
- All
Science Talk
- All
Amanda's Talks
- All
- Video Talk
- Featured
- 2016 Onwards
- 2011-2015
- 2010 and Earlier
- Science Talk
- Policy Talk
One-pager
- All
Music
- All
Amanda Feilding
- All
Events
- All
Highlights
- All
Psilocybin for Depression
- All
Current
- All
Category
- All
- Science
- Policy
- Culture
Substance/Method
- All
- Opiates
- Novel Psychoactive Substances
- Meditation
- Trepanation
- LSD
- Psilocybin
- Cannabis/cannabinoids
- Ayahuasca/DMT
- Coca/Cocaine
- MDMA
Collaboration
- All
- Beckley/Brazil Research Programme
- Beckley/Maastricht Research Programme
- Exeter University
- ICEERS
- Beckley/Sant Pau Research Programme
- University College London
- New York University
- Cardiff University
- Madrid Computense University
- Ethnobotanicals Research Programme
- Freiburg University
- Medical Office for Psychiatry and Psychotherapy, Solothurn
- Beckley/Sechenov Institute Research programme
- Hannover Medical School
- Beckley/Imperial Research Programme
- King's College London
- Johns Hopkins University
Clinical Application
- All
- Depression
- Addictions
- Anxiety
- Psychosis
- PTSD
- Cancer
- Cluster Headaches
Policy Focus
- All
- Policy Reports
- Advisory Work
- Seminar Series
- Advocacy/Campaigns
Type of publication
- All
- Original research
- Report
- Review
- Opinion/Correspondence
- Book
- Book chapter
- Conference abstract
- Petition/campaign
Search type